Ever wondered who’s behind the scenes, ensuring your medical bills are accurate and your health insurance runs smoothly? Meet the Medical Coder, an unsung hero in the healthcare industry. Stay tuned as this article delves into their world, unraveling their roles, responsibilities, and the impact they have on your healthcare journey.
Who Are Medical Coders?
Medical coders use standardized codes to document patient records, diagnoses, procedures, and services. These codes are essential for maintaining accurate patient records and ensuring proper billing. Without medical coders, healthcare providers would struggle to navigate complex billing and insurance processes.
Their role extends beyond simple data entry, requiring a strong understanding of medical terminology and coding systems. Coders work in various healthcare settings, such as hospitals and insurance companies. Their meticulous attention to detail ensures that medical documentation is precise and compliant with industry standards.
Role of a Medical Coder
Medical coders act as a vital link between healthcare providers, insurance companies, and regulatory bodies. They ensure that medical records are properly coded to facilitate accurate billing and reimbursement. By maintaining coding accuracy, they help prevent financial losses and legal issues for healthcare facilities.
Apart from assigning codes, coders also conduct audits and collaborate with healthcare professionals. Their role demands continuous learning to stay updated with changing medical guidelines. As a result, they play a crucial part in maintaining efficiency within the healthcare system.
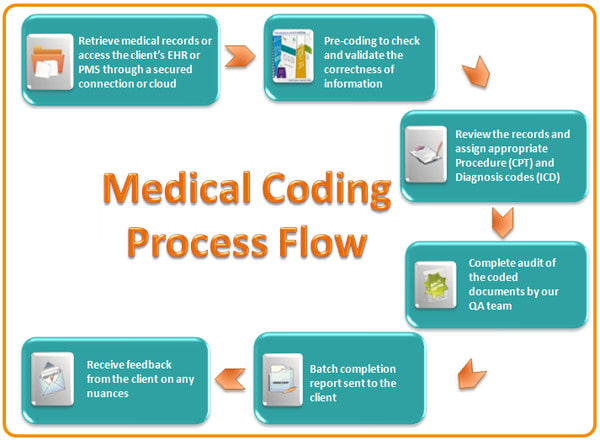
Code Assignment in Medical Coding
One of the key responsibilities of a medical coder is accurately assigning codes for medical services. They analyze clinical documentation to determine the correct codes for diagnoses, treatments, and procedures. These codes help streamline billing processes and standardize medical data across healthcare facilities.
Errors in code assignment can lead to claim denials and financial losses for medical institutions. Therefore, coders must have a deep understanding of classification systems like ICD and CPT. Their expertise ensures that medical services are accurately represented in patient records and insurance claims.
Accuracy and Compliance in Medical Coding
Accuracy is critical in medical coding, as even minor mistakes can result in claim denials and legal complications. Coders must thoroughly review medical records to ensure that assigned codes align with the provided documentation. Their precision is essential for maintaining the integrity of patient records.
Compliance is another crucial aspect of medical coding, requiring adherence to strict healthcare regulations. Coders must stay updated with coding changes and legal requirements, such as HIPAA. By ensuring compliance, they help protect patient confidentiality and avoid fraudulent billing issues.
Data Quality Improvement in Medical Coding
Medical coders contribute to data quality by ensuring accurate and complete documentation. High-quality coding allows for efficient billing, proper insurance processing, and accurate patient care records. Their role also supports medical research by providing reliable healthcare data.
Beyond coding, they identify discrepancies in medical records and work with providers to correct them. This improves the overall reliability of health data used for patient care and research. Their efforts enhance operational efficiency and the accuracy of medical statistics.
Communication and Collaboration in Medical Coding
Medical coders work closely with physicians, billing specialists, and insurance representatives. Effective communication ensures that patient records are clear and coding errors are minimized. Their role involves resolving discrepancies in documentation to prevent claim rejections.
Collaboration is essential in maintaining a smooth billing process and regulatory compliance. Coders participate in team discussions, provide guidance on documentation, and share updates on coding changes. Their teamwork helps optimize the efficiency of healthcare operations.
Adaptation to Coding Changes
The medical coding industry constantly evolves, requiring coders to adapt to new coding systems and regulations. Frequent updates in ICD and CPT codes demand continuous learning and training. Coders must stay informed to prevent errors and ensure accurate billing.
Adapting to coding changes is essential for maintaining compliance with healthcare laws. Many coders pursue additional certifications and attend workshops to enhance their skills. Their ability to adapt ensures a smooth transition when new coding updates are introduced.
Final Thoughts
Medical Coders are essential to the healthcare industry, ensuring the accuracy of medical documentation and financial transactions. Their role supports patient care, insurance claims, and medical research while maintaining compliance with healthcare regulations. The job requires meticulous attention to detail and continuous learning, making it a challenging but rewarding career.
Frequently Asked Questions
What skills are needed to become a Medical Coder?
A Medical Coder needs strong analytical skills, attention to detail, knowledge of medical terminology, and expertise in coding systems like ICD and CPT.
How long does it take to become a Medical Coder?
Most Medical Coding programs take 6 months to 2 years to complete, depending on the level of certification and training.
Is Medical Coding a good career choice?
Yes! Medical Coding offers job stability, remote work opportunities, and competitive salaries, making it a great career path.
Do Medical Coders work from home?
Many Medical Coders work remotely, especially in billing departments or insurance companies, offering flexible career options.